Views: 0 Author: Site Editor Publish Time: 2025-08-05 Origin: Site
A hematology analyzer checks blood cells and helps doctors learn about health. It does a complete blood count by looking at red cells, white cells, and platelets fast. Hematology analyzers use machines to test samples quicker and make fewer mistakes. They help make blood tests more correct and trustworthy. Hospitals and labs use hematology analyzers to care for patients better.
Aspect | Impact |
|---|---|
Speed | Automated hematology analyzers can check up to 119 CBCs each hour. |
Accuracy | Automation lowers mistakes by up to 90%. |
Data Integration | They link to lab systems for easy reports and better workflow. |
Hematology analyzers count blood cells fast and correctly. This helps doctors find and watch health problems.
Three main technologies help study blood cells closely. These are impedance, flow cytometry, and optical methods.
There are different analyzer types. These are 3-part, 5-part, 6-part, and 7-part analyzers. Each type gives a different amount of detail. This helps clinics, hospitals, and labs pick what they need.
These machines help doctors find sickness, watch patients, and do research. They give good blood test results and can find blood problems early.
Picking the best analyzer depends on lab size, how many tests are needed, how much automation is wanted, and the budget. This helps make blood testing fast and correct.

Modern hematology analyzers use special tools to check blood. These tools help labs test blood fast and with few mistakes. They also make sure tests are done the same way each time. The three main tools are impedance, flow cytometry, and optical methods.
Impedance technology is important in many hematology analyzers. It checks changes in electric resistance when blood cells move through a tiny hole. This helps count and measure cells in blood.
Blood cells go one at a time through a small gap between two electrodes.
Each cell blocks some electric current and makes a small change called a "blip."
The analyzer counts these blips to know how many cells there are.
The size of each blip shows how big the cell is.
The analyzer makes charts to show cell sizes and numbers.
Impedance sorts cells by size, but it may not tell apart cells that look alike.
Impedance lets hematology analyzers work fast and test lots of samples. Studies show impedance can sort blood cell types and find changes from disease. It does not need extra dyes or chemicals. Some machines use impedance with other tools to get very good results, sometimes over 93% correct. This tool helps with quick testing and can be used right where care is given.
Note: Impedance-based hematology analyzers give good results for most blood tests. They may not work as well when cells are almost the same size.
Flow cytometry uses lasers and special dyes to study blood cells. It helps hematology analyzers find and count many kinds of cells, even rare ones.
The analyzer mixes blood with antibodies that stick to certain cell markers.
It adds a dye that sticks to DNA.
Red blood cells are taken out, leaving white blood cells and others to study.
The analyzer shines a laser on the cells as they pass by one at a time.
The machine records how each cell reacts to the light and dye.
It uses this data to sort and count different cell types like lymphocytes, monocytes, and neutrophils.
Flow cytometry can find rare cells and spot odd shapes. It often matches or beats hand counting for being correct. It also finds more reticulocytes than some other ways because it uses strong dyes. Flow cytometry works fast and can check thousands of cells in minutes. It helps doctors find sickness and watch treatment.
Tip: Flow cytometry in hematology analyzers gives quick, detailed results. It can find small changes in blood that other ways might miss.
Optical methods use light to look at blood cells. These methods help hematology analyzers see cell size, shape, and inside parts.
Optical light scatter checks how cells bend and reflect light. This shows cell size and granules inside.
Multi-Angle Polarized Scatter Separation (MAPSS™) uses many light angles to study cells closely.
Digital image analysis helps find odd cell shapes.
Optical diffraction tomography and deep learning can sort cells by how they bend light, without dyes.
These optical methods give fast and correct blood counts. They help hematology analyzers tell apart many cell types. Some systems use both optical and digital tools for better results.
Technology | What It Measures | Main Benefit |
|---|---|---|
Impedance | Cell size and count | Fast, label-free, high volume |
Flow Cytometry | Cell markers, DNA, cell types | Detailed, sensitive, specific |
Optical Methods | Size, shape, granules, structure | Accurate, rapid, visual |
Automated hematology analyzers use these tools to test many blood samples quickly. They help stop mistakes and make labs work better. These analyzers also have strong ways to check quality. Labs use steady control materials and patient samples to check if results are right. Regular checks help keep blood test results trustworthy.
A complete blood count gives doctors key facts about blood cells. Hematology analyzers check many important things in blood. These results help doctors find and watch health problems.
Red blood cells move oxygen from lungs to the body. Hematology analyzers count red blood cells and look at their size and shape. The number of red blood cells can show if someone has anemia or polycythemia. The normal amount depends on age and if you are male or female.
Age Group / Sex | RBC Count Reference Range (×10¹²/L) |
|---|---|
Adult Male | 4.20 – 6.00 |
Adult Female | 3.80 – 5.20 |
Pediatric (4–7 years) | 4.00 – 5.20 |
Neonate (0–1 days) | 4.10 – 6.10 |
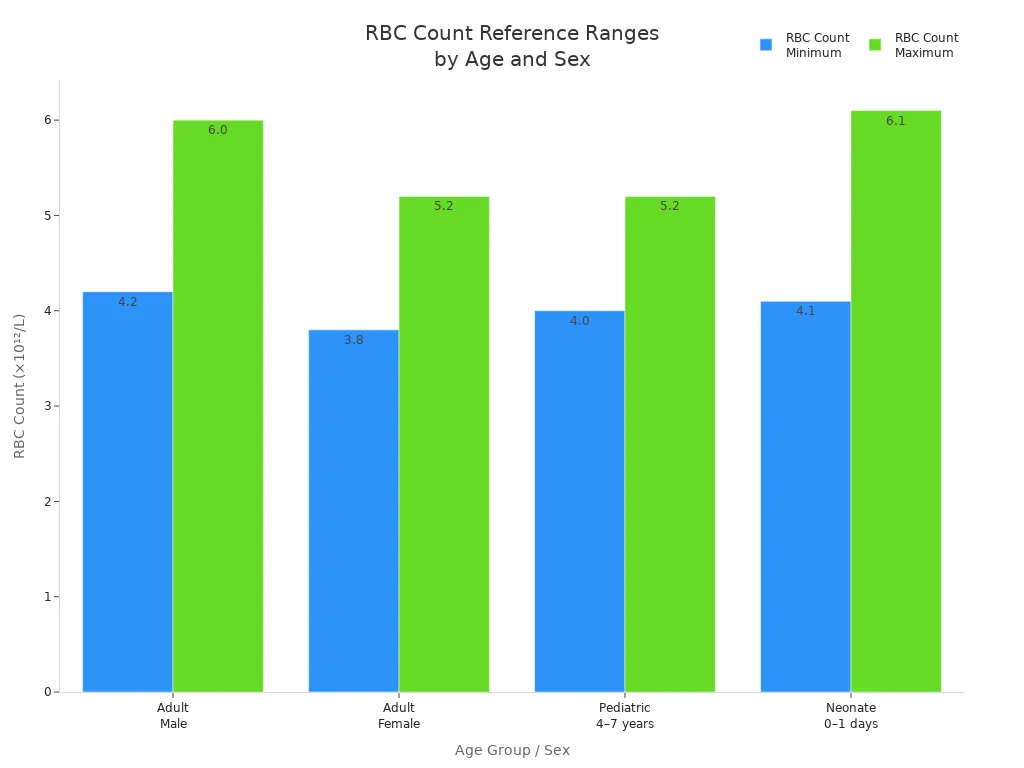
Hematology analyzers use pictures and artificial intelligence to spot odd red blood cell shapes. These shapes can mean diseases like sickle cell anemia or hereditary spherocytosis. The machine checks for elliptocytes, dacrocytes, acanthocytes, stomatocytes, spherocytes, hypochromic cells, and codocytes. This helps doctors find problems fast and means fewer hand checks.
Note: Changes in red blood cell number or shape often mean blood problems or long-term sickness. Doctors use these results to help choose treatment.
White blood cells keep the body safe from germs. Hematology analyzers count white blood cells and sort them into groups. The differential leukocyte count shows how many neutrophils, lymphocytes, monocytes, eosinophils, and basophils there are. Some machines also count immature granulocytes and nucleated red blood cells.
Hematology analyzers use electric impedance, light scatter, and fluorescence to tell white blood cell types apart.
Machine learning and deep learning make results better by checking things like nucleus shape and color.
The five-part differential helps doctors find infections, swelling, and blood cancers.
Strange results get a flag so someone can check by hand.
Doctors use white blood cell results to find infections, check immune health, and watch diseases like leukemia. Automated counts are quick and correct, but rare or strange cells may need a closer look under a microscope.
Platelets help stop bleeding by making clots. Hematology analyzers count platelets and check their size. The normal platelet count is 150–450 x 10⁹/L for most adults. This number is the same for men and women.
Source / Context | Normal Platelet Count Range (x10^9/L) | Notes |
|---|---|---|
Most Western labs (general) | 150 - 400 or 150 - 450 | Standard reference interval regardless of age, sex, ethnicity |
WHO diagnostic criteria for chronic myeloproliferative neoplasms | ≥ 450 | Major criterion for essential thrombocythemia |
JAMA Diagnostic Test Interpretation | 150 - 450 | Widely accepted normal range |
Thrombocytosis definition (literature consensus) | ≥ 450 | Threshold for clinically significant thrombocytosis varies but 450 is generally accepted |
Population distribution | 150,000 - 450,000/µL | Normal adult range, ~2.5% exceed upper limit |
Low platelets can make bruising or bleeding happen easily. High platelets may mean swelling, infection, or blood problems. Doctors use platelet counts to find things like immune thrombocytopenic purpura, myelodysplastic syndrome, and heparin-induced thrombocytopenia.
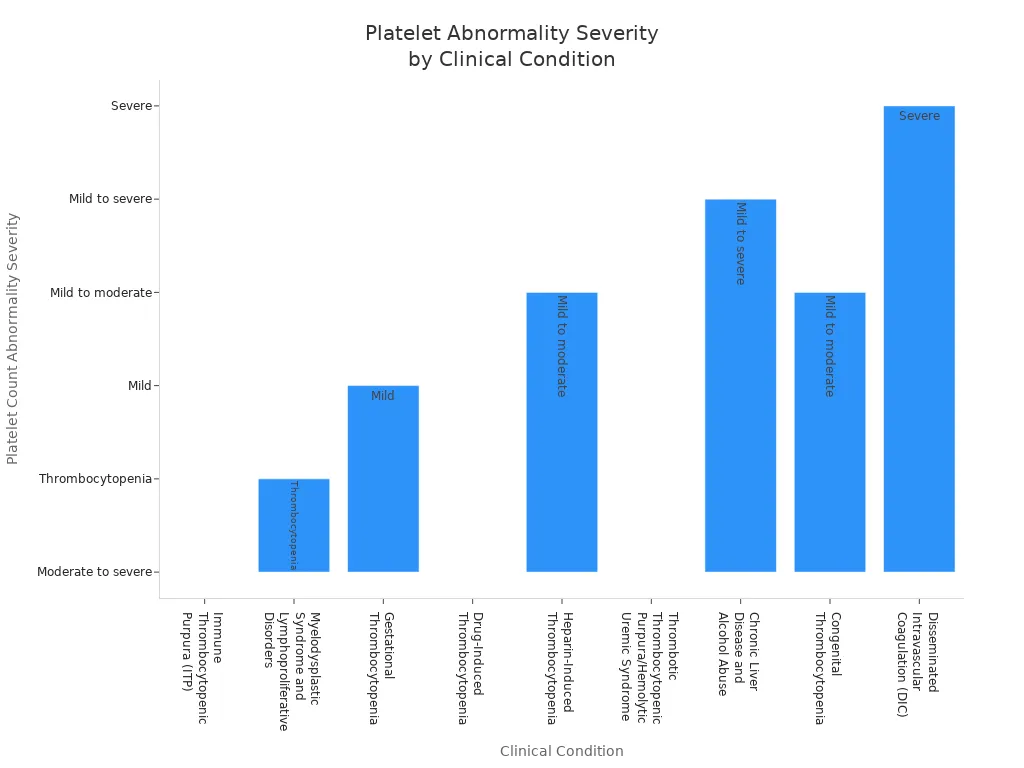
Tip: Changes in platelet count often mean bleeding problems, bone marrow trouble, or medicine side effects.
Hemoglobin shows how much oxygen blood can carry. Hematology analyzers measure hemoglobin with light, using methods like cyanmethemoglobin or SLS-Hb. These ways use light to check hemoglobin levels. Hematocrit is the part of blood made up of red blood cells. The analyzer figures out hematocrit from red blood cell count and size.
Hemoglobin is the main test for anemia. Doctors use special cutoffs for age and sex. Hematocrit helps find the cause of anemia and supports the diagnosis. These results help doctors treat and watch recovery.
Note: Low hemoglobin or hematocrit means anemia. High numbers may mean dehydration or polycythemia.
Advanced hematology analyzers check more than just basic counts. They look at reticulocytes, nucleated red blood cells, and platelet indices. These extra tests help doctors find problems early.
Marker Category | Specific Markers Measured by Advanced Hematology Analyzers |
|---|---|
Red Blood Cell Parameters | Reticulocytes (percentage and absolute count), Reticulocyte hemoglobin (RETIC-HGB), Nucleated red blood cells (nRBC, when presence suspected) |
White Blood Cell Parameters | True five-part white blood cell differential, Band neutrophils (when presence suspected) |
Platelet Parameters | Platelet count, Platelet distribution width, Mean platelet volume, Plateletcrit |
Reticulocytes show if the bone marrow makes enough new red blood cells.
Nucleated red blood cells can show up in bad anemia or in newborns.
Platelet indices help find bleeding risks or bone marrow problems.
Some analyzers use laser flow cytometry and optical fluorescence for these tests. The results give a full view of blood health. Doctors use these results to find anemia, leukemia, and other blood diseases. Artificial intelligence now helps study these markers, predict disease, and guide treatment.
3-part analyzers give simple blood cell results. They sort white blood cells into three groups. These are lymphocytes, monocytes, and granulocytes. The machines also measure red blood cells, hemoglobin, platelets, and total white blood cells. Many small clinics use them for regular health checks. They cost less money and do not need much care. These analyzers are easy to use. But they cannot tell all white blood cell types apart. This makes them less useful for hard cases.
5-part analyzers give more detailed results than 3-part ones. They split white blood cells into five types. These are neutrophils, lymphocytes, monocytes, eosinophils, and basophils. These analyzers check over 20 blood facts, like mean cell volume and mean platelet volume. They help doctors find infections, allergies, and blood cancers. Hospitals and big labs pick these machines for better accuracy and more features. They need more care and trained workers.
6-part analyzers add immature granulocyte counts to the five-part system. This extra detail helps doctors find bad infections and sepsis early. Cancer centers and special labs use them to watch patients during chemotherapy. 7-part analyzers go even further. They check special markers like reticulocytes and nucleated red blood cells. These machines give the most complete blood check. They help with research and hard disease cases but cost more and need regular care.
Analyzer Type | WBC Differentiation | Key Features | Advantages | Disadvantages | Typical Use Cases |
|---|---|---|---|---|---|
3-Part | 3 broad groups | Basic diagnostics | Affordable, simple | Limited precision | Small clinics |
5-Part | 5 types | Detailed CBC, >20 parameters | High accuracy | More maintenance | Hospitals, labs |
6-Part | 5-part + IG | Adds IG count | Enhanced diagnostics | Complex, costly | Oncology, advanced labs |
7-Part | 6-part + special markers | Most comprehensive | Superior insights | Premium price | Research labs |
Point-of-care hematology analyzers give fast results near the patient. They use small blood samples and work well in clinics or emergency rooms. These machines help doctors make quick choices and improve care. They also cut down the time patients wait. Benchtop models stay in labs and test more samples at once. They have more features and better accuracy for big hospitals. Both types give good blood tests, but point-of-care models focus on speed and easy use.
Tip: Point-of-care analyzers help when time is short. Benchtop models are best for busy labs that need detailed results.
Hematology analyzers are important for finding blood problems. They help doctors find out what is wrong fast. The machine checks blood for changes in red cell count, white cell count, platelet count, and hemoglobin concentration. It can help spot anemia, bacterial infections, viral infections, and leukemia. Doctors use the results to see if someone has thrombocytopenia or thrombocytosis. The analyzer also helps find allergic reactions and parasitic infections. It can show patterns that help doctors tell if an infection is viral or bacterial. The analyzer finds rare blood diseases by looking at cell shapes and sizes. It also finds problems with platelet count, which helps doctors diagnose things like disseminated intravascular coagulation and microangiopathic hemolysis.
Common conditions diagnosed using hematology analyzers:
Anemia
Bacterial infections
Viral infections
Leukemia
Platelet disorders
Allergic reactions
Parasitic infections
Doctors use blood screening and CBC results to help choose treatments.
Doctors use hematology analyzers to watch patients over time. The machine checks blood changes during treatment. It looks at platelet count, hemoglobin concentration, and other cell numbers. Hospitals use these results to see if medicine is working. The analyzer helps find problems early, like infections or bleeding. New machines give fast results, so doctors can act quickly. Some hospitals use wearable devices for real-time checks. These devices send alerts if blood changes suddenly. The analyzer flags abnormal results so staff can check them. It helps teams care for patients in hematology and oncology.
Ways hematology analyzers support monitoring:
Automated testing for quick results
Continuous tracking of platelet count and hemoglobin concentration
Alerts for abnormal blood results
Data management for easy review
Researchers use hematology analyzers to study blood diseases. The machine helps them learn how blood cells change when someone is sick. It checks platelet count, hemoglobin concentration, and cell types. Scientists use the results to test new treatments. The analyzer helps find patterns in blood that show how a disease is getting worse or better. It supports studies on rare blood disorders. Researchers use blood screening to collect data for big studies. The analyzer gives reliable results, which helps make diagnostic testing and patient care better.
Application | How Hematology Analyzers Help | Key Parameters Checked |
|---|---|---|
Diagnosis | Finds blood disorders | Platelet count, hemoglobin concentration, cell types |
Monitoring | Watches patient progress | Platelet count, hemoglobin concentration, CBC results |
Research | Helps with disease studies | Platelet count, hemoglobin concentration, blood screening |
Labs need to pick analyzers that fit their work. Small clinics often use benchtop analyzers. These can test 30 to 50 blood samples each hour. Big hospitals need machines that test 100 or more samples every hour. Pediatric labs want analyzers that use tiny blood samples, as little as 10 to 20 microliters.
Some important things to think about are:
How many tests the lab does each day
If the patients are adults, kids, or both
How much blood is needed for each test
If the analyzer works with lab computer systems
How much space the analyzer needs and how it fits in the lab
If the company offers help and supplies
Labs with lots of patients need fast analyzers that can grow with them. Smaller labs like simple and cheaper machines. How often the analyzer needs fixing or checking also matters.
Lab Type | Throughput Needed | Sample Volume | Preferred Analyzer Features |
|---|---|---|---|
Small Clinic | 30–50/hr | 100–200 µL | Compact, easy maintenance |
Pediatric Center | 30–100/hr | 10–20 µL | Microsampling, gentle handling |
Large Hospital | 100+/hr | 100–200 µL | High automation, LIS integration |
Tip: Labs should look at who their patients are and how many samples they get each day before picking an analyzer.
Automation helps labs work better and make fewer mistakes. New analyzers do things like label samples and enter data by themselves. They use barcodes to keep track of samples and make sure results are right. Automation makes testing faster and lets labs test more samples. Workers can spend more time on hard cases while machines do the easy jobs. Connecting analyzers to lab computers makes handling data simple.
Some good things about automation are:
Fewer mistakes from people
Faster test results
Samples are easy to track
Less work for staff
Smart help from AI
Callout: Automated analyzers make labs more accurate and help them work faster.
Rules and money are big parts of picking an analyzer. Labs must follow rules like HL7 so data moves easily between systems. Special settings and reports help labs check quality. Keeping track of data helps labs follow the rules.
The price is more than just buying the analyzer. Labs also need to think about:
The cost of supplies and controls
Money for fixing and checking the analyzer
Warranties and upgrades to protect against big costs
Training workers and updating instructions
Extra costs if the lab gets bigger later
Labs can buy new, used, or rent analyzers. Used ones are cheaper but need to be checked well. Renting spreads out the cost and often includes repairs.
Taking care of analyzers with regular checks and training helps them last longer. Using technology helps labs watch supplies and see how well analyzers work.
Cost Factor | Description |
|---|---|
Reagents & Controls | Ongoing expenses, vendor or third-party |
Service Contracts | Coverage for calibration, repairs |
Warranty & Upgrades | Protection against major expenses |
Training | Staff time for onboarding, SOP updates |
Scale-up Costs | Future expansion needs |
Note: Labs should think about the first cost, what they will keep paying, and the rules they must follow to do well for a long time.
A hematology analyzer gives quick and correct blood test results. It helps doctors decide how to care for patients. Knowing about hematology tools and types makes labs work better. New technology brings AI, machines that work by themselves, and small devices. These updates help doctors find and treat sickness faster.
Future changes in hematology analyzers:
AI helps spot problems and makes work easier
Faster and smaller machines are coming
Tests will be more exact and use cloud data
Key Parameter | Clinical Contribution |
|---|---|
RBC, WBC, Platelets | Help doctors find sickness, watch health, and plan care |
Labs should pick a hematology analyzer that meets their needs now and can grow with them later.
A hematology analyzer looks at blood cells. It helps doctors find out if someone is sick. It gives quick results for red cells, white cells, and platelets. Labs use it to help check and watch for diseases.
Most new analyzers are right more than 90% of the time. They use smart technology and get checked often. Labs trust these machines to give good blood counts.
A hematology analyzer cannot say if someone has cancer. It can find strange blood cells or numbers. Doctors use these results to see if more tests are needed.
Labs should follow what the maker says. Most analyzers need cleaning every day and checks each month. Regular care keeps results right and helps the machine last longer.
Analyzer Type | WBC Groups Counted | Main Use |
|---|---|---|
3-Part | 3 | Basic screening |
5-Part | 5 | Detailed testing |
A 5-part analyzer gives more facts about white blood cells. It helps doctors find more kinds of blood problems.


